
เทคนิคการแปลงเพศ
หมอเชฏฐวุฒิ ให้สวยเหมือนธรรมชาติ
Gender affirmation surgery at WIH International Hospital, Bangkok, Thailand
Gender affirmation surgery is a procedure that helps people transition to their self-identified gender.
Gender affirming surgery is known by numerous other names, including gender-affirmation surgery, sex reassignment surgery, gender reassignment surgery, sex change surgery and gender confirmation surgery.
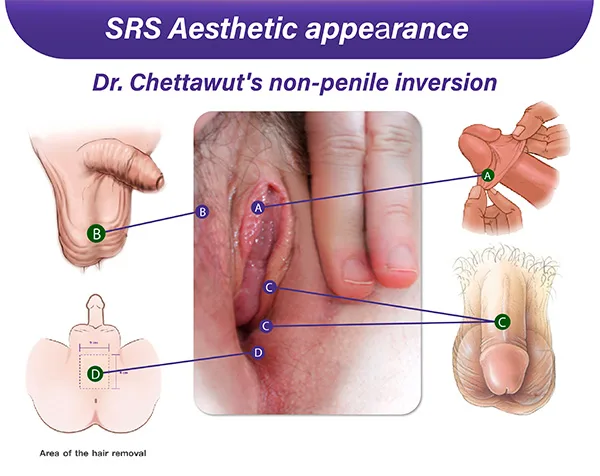
Dr. Chettawut’s non-penile inversion technique is well known as a top option for gender affirmation surgery, particularly among transgender women worldwide. This method produces the best aesthetic appearance of the vulva, commonly the priority of patients’ desire.
The non-penile inversion technique is more adaptable and flexible than the obsolete penile inversion technique. In the traditional penile inversion technique, most penile skin is inverted inside the vagina to serve as the lining. The penile skin is also used to create the inner labia, so it must be stretched. This is a drawback, as using one material for different parts compromises the aesthetic result of the external genitalia. With the non-penile inversion technique, the penile skin is no longer inverted into the vagina, which is more beneficial as it can be freely managed. It can be maximized, pulled, and stretched adequately to achieve a vertically oriented vulva. The approach includes careful placement of skin and tissue to mimic the contours and features typical of female genitalia, contributing anatomically correct surgical outcomes in a single-step procedure.
Why is the aesthetic appearance of the external genitalia so crucial following gender affirmation surgery?
With Dr. Chettawut’s non-penile inversion technique, the desired aesthetics that are as close as a cis female’s vulva can be achieved. This plays a vital role in building self-confidence, body positivity, and general well-being from an emotional and psychological aspect. It also fosters a stronger sense of self-assurance and a smoother integration into a person’s affirmed gender role.
The vulva is the part of your genitals on the outside of your body. It includes your labia, clitoris, vaginal opening, and the opening to the urethra.
The critical parts of the vulva are the inner and outer labia, clitoris, urethral and vaginal opening.
A) Clitoris:
This is the vulva’s most sensitive, or erogenous, zone. The clitoris is placed underneath the clitoral hood and designed to bend anteriorly away from the pubis, as is the natural alignment in a biological woman.
The clitoris is made from the most sensitive part of the glans penis that transmits erotic sensation from the innervation of the dorsal nerve of the clitoris.
B) Inner labia:
The inner labia, also known as the labia minora, are a pair of small, delicate, and elongated folds of skin located within the outer labia (labia majora) of the female genitalia. They are on either side of the vaginal opening and enclose the clitoral hood and clitoris. The appearance of the inner labia can vary widely from person to person, and there is a natural diversity in size, shape, color, and texture. The length and size of the inner labia can vary depending on the condition of the foreskin, which is different between circumcised and uncircumcised patients.
Dr. Chettawut uses a part of the foreskin (prepuce) for the inner side, which is labeled A, and the penile skin for the outer side, which is labeled C, to form the lip-like appearance of the inner labia. The constructed inner labia have a lot of sensory nerve endings, which contribute to sexual pleasure. The coloration of the inner labia can be light pink for those who have originally pink penile foreskin (prepuce).
C) Outer labia:
The outer labia, or labia majora, are the two folds protecting the urethral and vaginal opening. This is usually fleshy and has fat tissue underneath. This part is made of the skin from the scrotum.
D) Urethral Opening:
The urethral opening is positioned just above the vaginal opening, allowing the usual urination pattern. The total removal of surrounding spongy tissue called corpus spongiosum is an essential step during urethral opening reconstruction to prevent the engorgement of the tissue under the urethra during sexual arousal.
The bulging under the urethral opening from either the remnant corpus spongiosum or the fold of inverted penile skin (from the traditional penile inversion technique) compromises the aesthetic look of the vulva. It may cause a narrowing of the vaginal opening.
E) Vaginal Opening:
The vaginal introitus (vaginal entrance) is the entrance to the vagina, encompassing the distal end of the penile skin flap, which is labeled C as the bilateral side wall, and the perineal skin flap, which is labeled D as the floor of the vaginal entrance.
Dr. Chettawut emphasizes that the form of the reconstructed vaginal opening must have a vertical orientation, similar to the shape of a cis female’s vaginal opening.
23 years old SRS patient from Poland
Example result of Dr. Chettawut’s Non-penile inversion for gender affirming surgery
This case shows a typical result of Dr. Chettawut’s non-penile inversion technique for those with average penile length (without a circumcision).
The labia minora was constructed using the whole penile and prepuce skin to form the lip-like fold starting from the clitoral frenulum down to the sides of the vaginal opening.
In the second picture, where the labia were spread apart, the vaginal opening (made using the non-penile inversion technique) is vertically elongated or has an oval shape as it usually appears in a biological woman (not too broad or big like a hole).
The urethral opening appears anatomically correct in location and size.
The labia majora looks proportionate and beautiful without any noticeable scarring. The shape, size, and proportion of the labia majora matched the patient’s body.
Overall, this 2-month post-op photo depicts a positive result with normal to rapid external genital healing. The patient reported no difficulty doing her vaginal dilation routine and maintained her 6.5 inches vaginal depth.
![WIH INTERNATIONAL HOSPITAL [TH]](https://wihhospital.com/th/wp-content/uploads/2022/05/wih-logo-color.png)